Lung MRI
“To boldly go where most sequence developers have not gone before…”. Imaging empty space, i.e. air, is impossible by standard MRI and notably lung tissue is built from mesoscopic tissue cavities filled with air. Unfortunately, these cavities also lead to a very rapid signal decay and what is left in the basket disappears much faster than in any other tissue. As if this would not be enough, there is motion everywhere: motion due to natural breathing and motion due to the beating heart. Evidently, MRI of the lung is one of the most challenging tasks that you can think of and likely represents the royal path to MR sequence development.
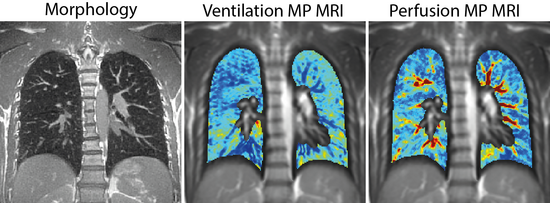
We offer dedicated MRI technology for functional, structural and tissue relaxometry lung imaging in the clinical setting with unprecedented resolution and specificity. For functional imaging we acquire a time series of two-dimensional chest images from which ventilation and perfusion information can be retrieved. In contrast, structural imaging is typically performed in 3D in either breath-hold or free-breathing. Further, we offer dedicated imaging strategies for lung tissue relaxometry and oxygen enhanced MRI, as well as automatized pipelines for pulmonary data analysis.
Currently, our methods are used at the Inselspital - University Hospital Bern, Charité - Universitätsmedizin Berlin, Universitäklinikum Heidelberg
Project leader and contact
Project members
Collaborators
- Prof. Dr. med. Philipp Latzin – Inselspital – University Hospital Bern
- Prof. Dr. med. Lukas Ebner – Inselspital – University Hospital Bern
- Prof. Dr. Dr. med. Adrian Huber – Inselspital – University Hospital Bern
- Dr. med. Sylvia Nyilas – Inselspital – University Hospital Bern
- Prof. Dr. med. Mark Wielpütz – Universitäklinikum Heidelberg
- Prof. Dr. med. Markus Mall – Charité - Universitätsmedizin Berlin
- Dr. med. Felix Döllinger – Charité - Universitätsmedizin Berlin
