In SEA2 SpineBot: Spinal Impedance Measurement Device
Adolescent idiopathic scoliosis (AIS) is among the most frequent musculoskeletal deformities in young individuals, significantly impairing a patient's mobility and overall health. In severe cases, different surgical treatment strategies involving invasive and irreversible vertebra fusion are performed. Currently, the decision on the treatment is grounded on empirical data from clinical studies and the surgeon's experience with the main challenge of finding a balance between the patient's mobility and structural stability while minimizing the risk of complications and follow-up treatments.
The biomechanical properties of deformed spines may help in the decision-making. However, the underlying data for this branch of research is based mainly on spinal loading simulator (SLS) experiments conducted in vitro. Furthermore, such spine segments originate from elderly individuals and are isolated from the body. Therefore, they do not represent the pathology of interest, nor is the surrounding tissue (e.g., ligaments and muscles) considered. The lack of in vivo biomechanical data on patients with AIS limits the development of novel treatment strategies and surgical approaches.
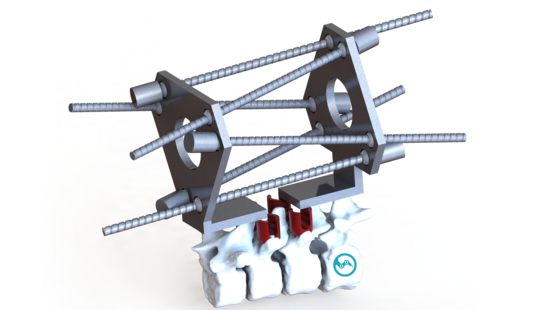
Based on a previous design (The Spinebot—A Robotic Device to Intraoperatively Quantify Spinal Stiffness | J. Med. Devices | ASME Digital Collection), we are developing a 6 DoF robotic measurement device (in SEA2 SpineBot) capable of assessing the Stiffness/Impedance to deflection ratio of a Functional Spinal Unit (FSU) in three planes. In addition, we are currently building up a Pre-interventional planning tool to process low-dose CT data to patient-specific robot motion and facilitate the integration of the biomechanical data in FE simulation. The "in SEA2 SpineBot" System will bridge conventional SLS with precise patient-specific planning for realistic in vivo measurement, pushing AIS treatment and spine research forward.
This PhD-Project is a collaboration between the BIROMED-Lab at the University of Basel, the Orthopedics Group of the University Children's Hospital of Basel | UKBB, and the Computational Bioengineering Group at the University of Berne.
Project leader: Dr. Lauren Chee Felix Erb Aysegül Kilic
Collaborators: PD Dr. Daniel Studer Prof. Dr. Carol-C. Hasler Prof. Dr. Philippe Büchler